Emergency department visits are slowly rising following the outbreak and immediate impact of the pandemic.
Emergency visits still down but slowly moving to pre-COVID levels
July 20, 2020
by John R. Fischer, Senior Reporter
Visits to emergency departments were 25% below pre-COVID-19 volumes at the end of June and are slowly picking up, according to TransUnion Healthcare, a subsidiary of information and insights company, TransUnion.
Driving this rebound are patients with high-acuity medical issues, who are returning to EDs at a faster pace than those with low-acuity concerns. This pattern could potentially mark a change in medical treatment settings that could reduce healthcare costs for providers, patients and payers, according to Jonathan Wiik, principal of healthcare strategy at TransUnion Healthcare, who discusses the matter in his new book, Healthcare Evolution: Helping Providers Get Paid in an Era of Uncertainty.
"The emergency department represents one of the most expensive and inefficient settings of care," he told HCB News. "Due to challenges with the Emergency Medical Treatment and Labor Act (EMTALA) — which requires anyone presenting at an emergency department to be stabilized regardless of their ability to pay or health insurance coverage — and consumer understanding of the best level of care, often high-cost, high-resource interventions are provided when there are other lower-cost alternative settings available. Patient education and leveraging the appropriate tools to engage patients early in navigating their healthcare coverage, cost and payments are key to managing these challenges."
A lack of price transparency and the complexity of the current healthcare system in the U.S. leads patients to be unaware of the differences in cost associated with diverse venues of care, according to Wiik.
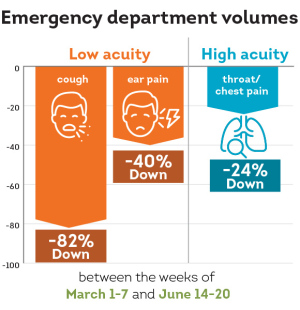
Adults with less acute diagnoses such as cough or ear pain are returning to the ED but at a slower pace, with visit volumes for both conditions down by 82% and 40%, respectively. Higher-acuity diagnoses such as throat and chest pain have been seen more, with visits 24% below pre-COVID-19 volumes.
Researchers determined their findings by evaluating patient admitting diagnoses within ED settings from March 1 – 7 and June 14 – 20 and observed patient volume visits at more than 500 U.S. hospitals between March 1 – 7 and June 21 – 27.
Looking at specific treatment settings, they found outpatient visit volumes to be down 7% during the week of June 21 – 27, having recovered 88% of volume lost since April 5 – 11, when volumes reached their lowest. For inpatient settings, visits were up by 75% since then and were 8% below pre-COVID-19 volumes. ED visits recovered 51% and were down 25%.
Visits by adults were higher than those of children in ED facilities, down 16% and 59% during the week of June 21 – 27, respectively. The same trend was seen in outpatient practices, with rates down by 5% and 34%. Visits from children at inpatient practices were slightly higher than those of adults, by 6% compared to 9%.
The cost of care in EDs is typically more expensive than that of medical clinics or telehealth alternatives. Anyone who shows up at an ED must be stabilized under the Emergency Medical Treatment and Labor Act regardless of whether they can pay or are covered under health insurance. This leads patients to receive treatments at one of the most expensive care sites in the U.S. healthcare system, even when their illness does not require it and often without a choice to go somewhere else after they arrive, says Wiik in his book.
In addition to contributing to greater costs for patients, these visits lead to overutilization of the ED, which, in turn, creates care delivery and affordability challenges and racks up almost $382 billion in wasted spending annually, according to a report by UnitedHealth Group.
Wiik, whose book offers strategies to all stakeholders and particularly healthcare providers for protecting their revenue and creating frictionless, positive patient experiences, says the industry needs a holistic, long-term strategy to curb healthcare costs.
"As potential shifts take place in healthcare settings, hospitals should focus on proactive engagement of patients in pre-service estimates and flexible payment options," he said. "Further, best-in-class financial clearance [options] are all must-haves in the post COVID-19 era."
TransUnion Healthcare defines pre-COVID-19 volumes as the average weekly visits measured during the first eight full weeks of the year, from the weeks of January 5 – 11 through February 23 – 29.
Healthcare Evolution: Helping Providers Get Paid in an Era of Uncertainty is now available to read.
Driving this rebound are patients with high-acuity medical issues, who are returning to EDs at a faster pace than those with low-acuity concerns. This pattern could potentially mark a change in medical treatment settings that could reduce healthcare costs for providers, patients and payers, according to Jonathan Wiik, principal of healthcare strategy at TransUnion Healthcare, who discusses the matter in his new book, Healthcare Evolution: Helping Providers Get Paid in an Era of Uncertainty.
"The emergency department represents one of the most expensive and inefficient settings of care," he told HCB News. "Due to challenges with the Emergency Medical Treatment and Labor Act (EMTALA) — which requires anyone presenting at an emergency department to be stabilized regardless of their ability to pay or health insurance coverage — and consumer understanding of the best level of care, often high-cost, high-resource interventions are provided when there are other lower-cost alternative settings available. Patient education and leveraging the appropriate tools to engage patients early in navigating their healthcare coverage, cost and payments are key to managing these challenges."
A lack of price transparency and the complexity of the current healthcare system in the U.S. leads patients to be unaware of the differences in cost associated with diverse venues of care, according to Wiik.
Adults with less acute diagnoses such as cough or ear pain are returning to the ED but at a slower pace, with visit volumes for both conditions down by 82% and 40%, respectively. Higher-acuity diagnoses such as throat and chest pain have been seen more, with visits 24% below pre-COVID-19 volumes.
Researchers determined their findings by evaluating patient admitting diagnoses within ED settings from March 1 – 7 and June 14 – 20 and observed patient volume visits at more than 500 U.S. hospitals between March 1 – 7 and June 21 – 27.
Looking at specific treatment settings, they found outpatient visit volumes to be down 7% during the week of June 21 – 27, having recovered 88% of volume lost since April 5 – 11, when volumes reached their lowest. For inpatient settings, visits were up by 75% since then and were 8% below pre-COVID-19 volumes. ED visits recovered 51% and were down 25%.
Visits by adults were higher than those of children in ED facilities, down 16% and 59% during the week of June 21 – 27, respectively. The same trend was seen in outpatient practices, with rates down by 5% and 34%. Visits from children at inpatient practices were slightly higher than those of adults, by 6% compared to 9%.
The cost of care in EDs is typically more expensive than that of medical clinics or telehealth alternatives. Anyone who shows up at an ED must be stabilized under the Emergency Medical Treatment and Labor Act regardless of whether they can pay or are covered under health insurance. This leads patients to receive treatments at one of the most expensive care sites in the U.S. healthcare system, even when their illness does not require it and often without a choice to go somewhere else after they arrive, says Wiik in his book.
In addition to contributing to greater costs for patients, these visits lead to overutilization of the ED, which, in turn, creates care delivery and affordability challenges and racks up almost $382 billion in wasted spending annually, according to a report by UnitedHealth Group.
Wiik, whose book offers strategies to all stakeholders and particularly healthcare providers for protecting their revenue and creating frictionless, positive patient experiences, says the industry needs a holistic, long-term strategy to curb healthcare costs.
"As potential shifts take place in healthcare settings, hospitals should focus on proactive engagement of patients in pre-service estimates and flexible payment options," he said. "Further, best-in-class financial clearance [options] are all must-haves in the post COVID-19 era."
TransUnion Healthcare defines pre-COVID-19 volumes as the average weekly visits measured during the first eight full weeks of the year, from the weeks of January 5 – 11 through February 23 – 29.
Healthcare Evolution: Helping Providers Get Paid in an Era of Uncertainty is now available to read.