Ultrasound and cone beam CT imaging can
ensure greater precision of radiation delivered to
treat cervical cancer
ensure greater precision of radiation delivered to
treat cervical cancer
Combining CT with other imaging may enhance radiotherapy precision
October 14, 2019
by John R. Fischer, Senior Reporter
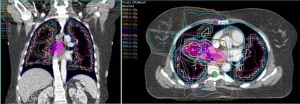
Combining CT scans with other forms of medical imaging may reduce the amount of healthy tissue exposed to radiation in radiotherapy procedures and subsequently minimize side effects.
That’s what researchers at the Institute of Cancer Research and the Royal Marsden NHS Foundation Trust are claiming. Divided into two groups, the researchers at both tested two imaging techniques that combine CT with ultrasound and SPECT to help form more efficient treatment plans for cases of cervical and lung cancers, respectively. They expect the combinations to create greater potential for more precise delivery of radiotherapy.
CT is often employed to determine how much tissue will be exposed to radiation, with a treatment plan drawn up and depicting margins around the tumor to ensure the whole mass is treated. These margins, however, expose healthy tissue to damaging radiation, leading to patients experiencing side effects after treatment.
This can especially be true when devising treatment plans for cervical cancer, which often include wide margins around the tumor to account for natural movements of the bladder and bowel that cause the tumor to shift position. In addition to side effects, women may not be able to complete treatment as a result.
To address this, the researchers propose using ultrasound, which is quick and effective for producing high-quality images, with cone beam CT, which can produce images that suit each patient’s anatomy each day when planning radiotherapy. The authors also point out that ultrasound is relatively cheap to perform and simple to incorporate into current radiotherapy practices.
Applied to 11 patients, the two modalities together produced more detailed images than either scan alone. The scans from each complemented one another by showing regions that were not visible on a single view, enabling clinicians to better outline the positions of the uterus and improve the precision of radiotherapy planning.
"Patients with cervical cancer receive radiation to the uterus and cervix. The position and shape of the uterus can vary greatly day to day and it is important we are able to visualize them for therapy," Dr. Emma Harris, leader of the Imaging for Radiotherapy Adaptation Team at the Institute of Cancer Research, told HCB News. "The uterus and cervix are easily visualized using ultrasound and therefore, are good candidate sites on which to test this technique. Other tumour sites that will benefit from this technology are prostate and liver. We are continuing to develop these techniques for cervix, liver and prostate."
The other proposal calls for combining SPECT with CT to help determine treatment plans for lung cancer. Patients with this disease often experience trouble breathing which can be made worse by the delivery of radiotherapy to the lungs, and lead to side effects such as disabling breathlessness. This makes it extremely important for doctors to limit the amount of normal lung tissue regions exposed to radiation.
SPECT, which produces computerized 3D scans by tracking and imaging the location of a radioactive tracer compound, can show certain body functions such as blood flow to tissues and organs. Scanning 48 patients with it, researchers were able to predict if a person’s lung function would deteriorate following radiotherapy based on how much lung tissue received radiation, even at low dose. Those who became breathless were found to have a larger volume of healthy lung tissue exposed to low dose radiation, while those who did not report increased trouble breathing were found with SPECT to have comparatively small regions of healthy lung exposed to radiation.
The researchers say that together, SPECT scans and standard CT may provide helpful insights for treatment of patients whose breathing is limited already before receiving radiotherapy, and help amend treatment plans to limit low dose radiation exposure to normal regions of lungs with good blood flow.
“The data from our study confirm a significant difference in dose–volume histograms between anatomic (defined on CT) and perfused lung (defined on perfusion SPECT) volumes,” said the authors in their study. “This is partly explained by technical differences in the acquisition of lung volume between the techniques, but shows the potential for using perfusion volumes as an independent “organ-at-risk” when determining radiotherapy dose scheduling.”
The study on cervical cancer was published in the International Journal of Radiation Oncology, Biology, Physics.
The study on lung cancer was published in The British Journal of Radiology.
That’s what researchers at the Institute of Cancer Research and the Royal Marsden NHS Foundation Trust are claiming. Divided into two groups, the researchers at both tested two imaging techniques that combine CT with ultrasound and SPECT to help form more efficient treatment plans for cases of cervical and lung cancers, respectively. They expect the combinations to create greater potential for more precise delivery of radiotherapy.
CT is often employed to determine how much tissue will be exposed to radiation, with a treatment plan drawn up and depicting margins around the tumor to ensure the whole mass is treated. These margins, however, expose healthy tissue to damaging radiation, leading to patients experiencing side effects after treatment.
This can especially be true when devising treatment plans for cervical cancer, which often include wide margins around the tumor to account for natural movements of the bladder and bowel that cause the tumor to shift position. In addition to side effects, women may not be able to complete treatment as a result.
To address this, the researchers propose using ultrasound, which is quick and effective for producing high-quality images, with cone beam CT, which can produce images that suit each patient’s anatomy each day when planning radiotherapy. The authors also point out that ultrasound is relatively cheap to perform and simple to incorporate into current radiotherapy practices.
Applied to 11 patients, the two modalities together produced more detailed images than either scan alone. The scans from each complemented one another by showing regions that were not visible on a single view, enabling clinicians to better outline the positions of the uterus and improve the precision of radiotherapy planning.
"Patients with cervical cancer receive radiation to the uterus and cervix. The position and shape of the uterus can vary greatly day to day and it is important we are able to visualize them for therapy," Dr. Emma Harris, leader of the Imaging for Radiotherapy Adaptation Team at the Institute of Cancer Research, told HCB News. "The uterus and cervix are easily visualized using ultrasound and therefore, are good candidate sites on which to test this technique. Other tumour sites that will benefit from this technology are prostate and liver. We are continuing to develop these techniques for cervix, liver and prostate."
The other proposal calls for combining SPECT with CT to help determine treatment plans for lung cancer. Patients with this disease often experience trouble breathing which can be made worse by the delivery of radiotherapy to the lungs, and lead to side effects such as disabling breathlessness. This makes it extremely important for doctors to limit the amount of normal lung tissue regions exposed to radiation.
SPECT, which produces computerized 3D scans by tracking and imaging the location of a radioactive tracer compound, can show certain body functions such as blood flow to tissues and organs. Scanning 48 patients with it, researchers were able to predict if a person’s lung function would deteriorate following radiotherapy based on how much lung tissue received radiation, even at low dose. Those who became breathless were found to have a larger volume of healthy lung tissue exposed to low dose radiation, while those who did not report increased trouble breathing were found with SPECT to have comparatively small regions of healthy lung exposed to radiation.
SPECT and CT can help determine treatment
for lung cancer patients whose breathing is
limited already prior to receiving radiotherapy
for lung cancer patients whose breathing is
limited already prior to receiving radiotherapy
The researchers say that together, SPECT scans and standard CT may provide helpful insights for treatment of patients whose breathing is limited already before receiving radiotherapy, and help amend treatment plans to limit low dose radiation exposure to normal regions of lungs with good blood flow.
“The data from our study confirm a significant difference in dose–volume histograms between anatomic (defined on CT) and perfused lung (defined on perfusion SPECT) volumes,” said the authors in their study. “This is partly explained by technical differences in the acquisition of lung volume between the techniques, but shows the potential for using perfusion volumes as an independent “organ-at-risk” when determining radiotherapy dose scheduling.”
The study on cervical cancer was published in the International Journal of Radiation Oncology, Biology, Physics.
The study on lung cancer was published in The British Journal of Radiology.